Thyroid conditions can often be misdiagnosed if optimal thyroid levels are not taken into account. The American Thyroid Association estimates 60 percent of those with thyroid issues are unaware of their condition. Often patients with “normal” lab values may still have symptoms leaving them feeling abnormal. This article talks about the difference between normal and optimal thyroid levels and the necessary tests that should be done to distinguish whether or not your client has a problem with their thyroid.
Some of these links are affiliate links, that means when you sign up or purchase from these links we may receive a small commission at no extra cost to you. Thyroid Nutrition Educators is also a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. Learn more about our disclosure statement.
What is the Thyroid Gland
The thyroid gland is a butterfly-shaped organ that lies at the base of the neck just under the voice box. These two “wing” lobes lie against and around the trachea and are connected by a narrow strip of tissue.
It is part of the endocrine system and is responsible for secreting the following hormones:
- Triiodothyronine (T3)
- Tetraiodothyronine (thyroxine or T4)
These substances are carried to every cell in the body. Cells use thyroid hormones for the following functions:
- Metabolism
- Digestion
- Weight management
- Regulate body temperature
- Growth
- Heart function
- Brain function
- Muscle function
How the Thyroid Works
Thyroid hormone production and secretion are controlled by the hypothalamus and the pituitary gland in the brain. The hypothalamus and pituitary gland work together in what is known as the hypothalamic-pituitary axis (HPT).
Hypothalamic-Pituitary Axis (HPT) Controls Thyroid Hormones
The hypothalamus will release thyroid-releasing hormone (TRH) which will stimulate the pituitary gland to secrete TSH. TSH is the catalyst for the production of hormones T3 and T4 from the thyroid gland.
TSH is also responsible for the growth of thyroid cells and enlargement of the thyroid known as goiter.
Thyroid Hormones: Triiodothyronine (T3)
Triiodothyronine, or T3, is the active form of thyroid hormone. The thyroid produces only 20 percent of T3. The other 80 percent comes from the conversion of T4 to T3 within various body cells including the heart, kidneys, and liver.
Thyroid Hormones: Thyroxine (T4)
Tetraiodothyronine, also known as thyroxine or T4 makes up more than 80% of the hormone secreted from the thyroid. When released into the circulation, it forms T3 through the process of de-iodination.
A Negative Feedback Loop Promotes TSH Production
T4 and T3 exert a negative feedback loop telling the pituitary to shift the levels of TSH depending on the amount of T4 and T3 present in the body:
- HIGH levels of T3/T4 result in a DECREASE of TSH
- LOW levels of T3/T4 result in an INCREASE of TSH

Finding Optimal Thyroid Levels with Thyroid Hormone Tests
A shift in thyroid hormone levels may indicate a thyroid condition. The problem is that typical thyroid range lab values are often not the best indicator of healthy thyroid numbers.
If your client is experiencing thyroid symptoms their “normal” thyroid levels could indicate something that may be happening with the thyroid.
Learning what is optimal thyroid levels is helpful to know if there is a problem with the thyroid.
Getting a comprehensive thyroid panel will give insight into the health of this gland. This includes the following tests:
- Thyroid Stimulating Hormone (TSH)
- Free Thyroxine (Free T4)
- Free Triiodothyronine (Free T3)
- Thyroid peroxidase (TPO) antibodies
- Thyroglobulin antibody (TG) antibodies
- Thyroid-stimulating immunoglobulin (TSI) Antibodies
- Thyroid binding inhibitory immunoglobulin (TBII) Antibodies
- Reverse Triiodothyronine (rT3)
- Thyroid Ultrasound
- Your client’s symptoms
Thyroid Stimulating Hormone (TSH) Tests
Thyroid-stimulating hormone levels are considered the primary test for detecting both subclinical and full-blown thyroid dysfunction for those with no history of hypothalamic and pituitary problems.
TSH uses include:
- Primary screening test for thyroid dysfunction
- Evaluation of thyroid hormone replacement therapy in patients with primary hypothyroidism
- Evaluation of suppressive therapy in patients with follicular cell-derived thyroid cancer
Medication Affects TSH Levels
Medications may interfere with the measurement of TSH and affect interpretation in the following ways:
- Preventing the absorption of T4
- Production and secretion of hormones
- Affect the function of the HPT axis
- Increase clearance
- Prevent the conversion of T4 to T3
Medications that affect TSH include:
- Biotin Supplements
- Calcium supplements
- Iron supplements
- Estrogens and Birth Control Pills
- Antacids
- Amiodarone
- Lithium
- Tyrosine kinase inhibitors
- Bexarotene
- Dopamine
- Octreotide
- Ipilimumab
- Phenytoin
- Carbamazepine
- Glucocorticoids
- Beta-blockers
TSH Fluctuations Indicate Abnormalities in the Thyroid
TSH fluctuates throughout the day with the lowest value in the late afternoon and highest value between midnight and 4 am. Variations of TSH up to 50% do not necessarily reflect a change in thyroid status proving TSH should not be evaluated alone when assessing the thyroid.
TSH levels will change when hypothyroidism and hyperthyroidism are developing.
When TSH Is Elevated
An elevated or HIGH TSH level means the pituitary gland is releasing its hormone TRH to get the thyroid to produce more thyroid hormone. The thyroid is UNDERACTIVE due to a problem affecting the thyroid.
In HYPOTHYROIDISM and Hashimoto’s TSH is elevated.
When TSH is Low
A LOW TSH means the pituitary gland feels there is too much thyroid hormone in the blood and will slow or stop releasing TSH. Thyroid production will then decrease. This means the thyroid is OVERACTIVE and is producing too much thyroid hormone.
HYPERTHYROIDISM and Graves’ disease will have low TSH levels.

TSH Ranges in Pregnancy
TSH varies throughout the pregnancy. During the first trimester, TSH will decrease but rarely goes under 0.1 mU/L. TSH will become normal in the second trimester. Use trimester-specific ranges for TSH to determine if possible. Otherwise follow the upper limits of the normal range:
- 1st trimester: 0.1-2.5 μIU/mL
- 2nd trimester: 0.2-3.0 μIU/mL
- 3rd trimester: 0.3-0.3 μIU/mL
“NORMAL” TSH Values Miss Thyroid Dysfunction
For many medical professionals, TSH is a golden standard for diagnosing and managing thyroid dysfunction. To them, a TSH range in the normal means the thyroid is performing optimally.
Most lab values show a NORMAL range of TSH to be between 0.5 to 5.5. So the results would be as follows:
A TSH of LESS than 0.5 would show an overactive thyroid or HYPERthyroidism.
A TSH GREATER than 5.0 indicated an underactive thyroid or HYPOthyroidism.
A normal TSH lab value means there could be no problem with the thyroid but this is not always the case.
A normal TSH is not normal at all and often can progress to thyroid disease. Many people with normal TSH levels still have symptoms of thyroid disorders.
Antibodies in Those With Normal TSH Lab Values
Those with TSH levels between 3.0 and 5.0 μIU/mL often are more likely to also have the presence of antithyroid antibodies and will often progress to thyroid disease.
Excluding those with goiter, antithyroid antibodies, and a family history of thyroid disease, the average level of TSH is 1.5 μIU/mL.
These normal TSH lab values need to be lowered for those who are still experiencing antibodies and symptoms.
Lowering the Upper Limit of TSH Has Been Met With Critique
Lowering the limit for TSH has been met with critique among conventional medicine.
This is due to the reliance on evidence from levothyroxine therapy. Most research indicates a lack of benefit from levothyroxine therapy at lower levels keeping the upper limit of TSH at 4.0 to 5.0 (depending on the laboratory) more reasonable.
This is short-sighted and does not take into account that like nutrition medication needs to be individualized and more research needs to be done.
The Rationale for Lowering The TSH Upper Limit Lab Value
Analysis of the data from the National Health and Nutrition Examination Survey III study has suggested that TSH levels may be estimated in older age groups unless an age-specific TSH range is used.
Another study of 766 individuals with negative antibodies, a normal thyroid ultrasound, and no evidence of thyroid disease determined the TSH reference range should be limited to an upper limit of 4.0 μIU/mL.
The research indicates African-Americans typically have lower TSH levels averaging around 1.18 μIU/mL making the normal reference range of TSH levels at 4 of 5 μIU/mL can be problematic ranges.
The distribution of TSH averages does not have the normal bell curve structure. Instead, there is a tail-end at the upper limits of normal. Applying the bell curve to the TSH distribution would make the upper limit for TSH be 2.5 μIU/mL.
Other bodies of science have found flaws in the current TSH levels and proposed a lower upper limit for TSH.
The National Academy of Clinical Biochemists indicated that 95 percent of individuals without thyroid disease have TSH concentrations below 2.5 μIU/mL.
A new reference range was defined by the American College of Clinical Endocrinologists to be between 0.3- 3.0 μIU/mL.
Use Optimal Thyroid Levels Instead of Normal TSH Lab Values
Functional medicine professionals feel the normal TSH lab range is too wide and an optional TSH range should be used instead. This runs between 0.5 and 2.5 μIU/mL. So the results would be:
A TSH of LESS than 0.5 would show an overactive thyroid or HYPERthyroidism.
A TSH GREATER than 2.0 indicated an underactive thyroid or HYPOthyroidism.
Optimal Thyroid Levels That Indicate A Healthy Thyroid
Functional medical practitioners have said optimal ranges should be between 1 and 2.0 μIU/mL for a healthy person not taking thyroid medications.
Optimal Thyroid Levels For those with Thyroid Conditions
Those with thyroid conditions and on medications should have a TSH between 0.5 and 2.0 μIU/mL.
Thyroid medications with artificial T3 may also suppress TSH levels.
TSH levels in thyroid patients were found to be altered over 24 hours when taking a medication with a T4/T3 combination compared with T4 alone.
TSH levels began to decline and were suppressed for up to five hours after taking the medication. After five hours TSH levels began to rise and were elevated until 13 hours and stabilized for the remaining time.
If your client is on thyroid medication with T3 be sure to have them take their medication after getting a blood test.
TSH Optimal Thyroid Levels
Normal TSH lab values are not optimal thyroid levels. Use the following optimal reference ranges:
- Level for a healthy thyroid: 1 and 2.0 μIU/mL
- Level for those on medication: 0.5 and 2.0 μIU/mL
- Level for the elderly on medication: 0.5 and 2.5 μIU/mL
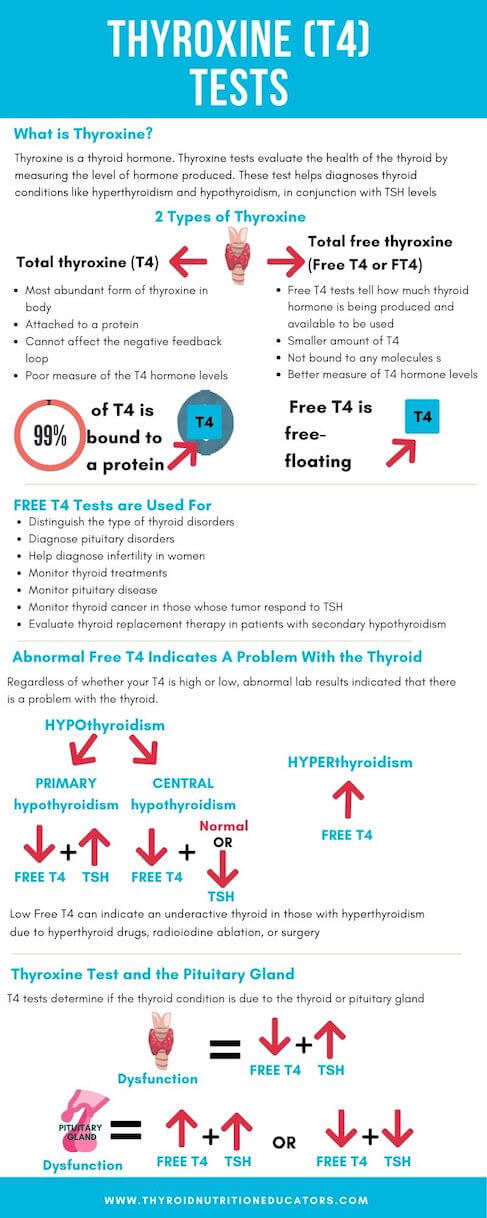
Thyroxine (T4) Tests
Thyroxine is a thyroid hormone. Thyroxine tests evaluate the health of the thyroid by measuring the level of hormone produced. This test diagnoses thyroid conditions like hyperthyroidism and hypothyroidism, in conjunction with TSH levels.
There are two types of Thyroxine:
- Total thyroxine (T4)
- Total free thyroxine (Free T4 or FT4)
Total thyroxine (T4)
Total thyroxine (T4) constitutes the most abundant form of thyroxine in the body. About 99 percent of T4 is bound to body proteins. This T4 is not metabolically available to affect the negative feedback loop.
Being attached to a protein it is affected by protein levels and is not an accurate measure of the T4 hormone.
Free Thyroxine (Free T4)
Free thyroxine or Free T4 tests can help to find how much thyroid hormone is being produced, hyper- or hypothyroidism.
Free thyroxine (Free T4 or FT4) is the smaller amount of thyroid hormone not bound to any molecules so it is free-floating.
Free T4 shows how much hormone is immediately available for the body to use which is why it is a better measure of hormone levels.
Free T4 is used to:
- Distinguish the type of thyroid disorders
- Diagnose pituitary disorders
- Help diagnose infertility in women
- Monitor thyroid treatments
- Monitor pituitary disease
- Monitor thyroid cancer in those whose tumor respond to TSH
- Evaluate thyroid replacement therapy in patients with secondary hypothyroidism
Regardless of whether your T4 is high or low, abnormal lab results indicated that there is a problem with the thyroid.
A low free T4 indicates hypothyroidism either primary when TSH is elevated or central when TSH is normal or low. It can also indicate an underactive thyroid in those with hyperthyroidism due to hyperthyroid drugs, radioiodine ablation, or surgery.
An elevated free T4 may indicate hyperthyroidism.
Thyroxine Test and the Pituitary Gland
T4 tests can also determine whether the thyroid condition resulted from a problem with the thyroid or the pituitary gland based on how much TSH is present at the time of the test.
LOW T4 could mean a thyroid or pituitary gland condition is responsible for hypothyroidism.
The thyroid is responsible if free T4 is LOW and the TSH is HIGH.
The pituitary gland is responsible if both free T4 and the TSH is either LOW or HIGH.
Thyroxine (T4) in Pregnancy
In pregnancy total T4 measurement is recommended as a way to monitor T4 levels. The changes in proteins may affect Free T4 and give a lower value than actually there.
Total T4 increases during the first trimester and the reference range is about 1.5 times that of nonpregnant women.
One study discovered the following T4 levels during pregnancy:
Free T4 Trimester Ranges:
- 1st Trimester: 0.8–1.53 ng/dL
- 2nd Trimester 0.7–1.20 ng/dL
- Third trimester: 0.7–1.20 ng/dL
Total T4 Trimester Ranges:
- 1st Trimester: 7.31–15.0 μg/dL
- 2nd Trimester: 8.92–17.38 μg/dL
- 3rd Trimester: 7.98–17.70 μg/dL
Free Thyroxine (Free T4) Optimal Thyroid Levels
Some health professionals feel that if your free T4 is not in the top half of the reference range means it is not a healthy number and could show signs of thyroid disruption. If your pituitary gland is the problem you want to work with your doctor to determine treatment options.
Standard Normal ranges of total free T4 are as follows:
- 9 – 23 pmol/L (0.7 – 1.8 ng/dL)
Optimal thyroid levels of free T4 are as follows:
- 15-23 pmol/L (1.2 – 1.8 ng/dL)
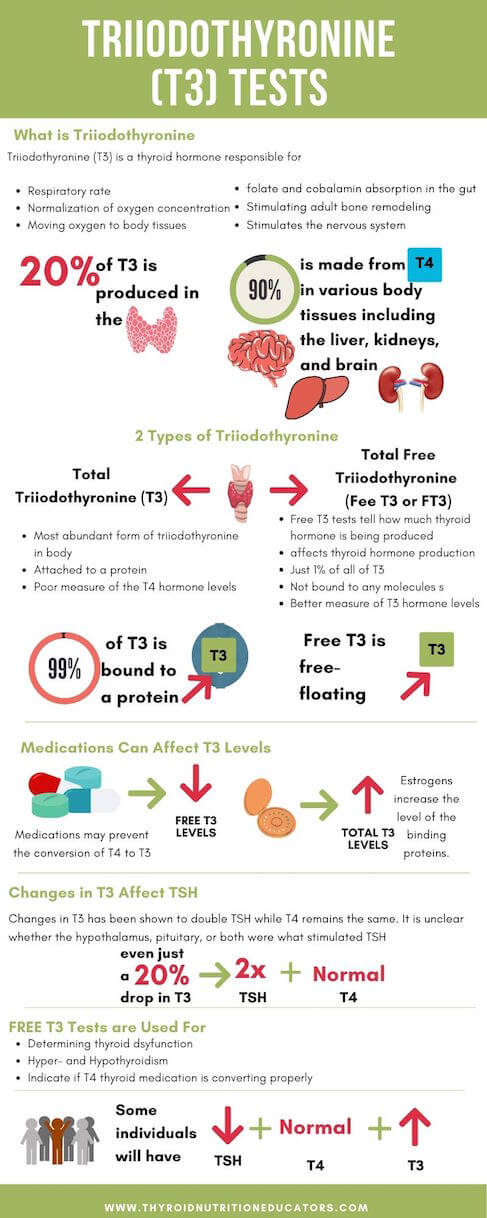
Triiodothyronine (T3) Tests
Triiodothyronine or T3 is another thyroid hormone that can be measured to determine thyroid dysfunction. Like T4, T3 is produced when the pituitary gland releases TSH.
Triiodothyronine (T3) Needed for Body Functions
T3 is responsible for the following:
- Respiratory rate
- Normalization of oxygen concentration
- Moving oxygen to body tissues
- Increasing folate and cobalamin absorption in the gut
- Stimulate adult bone remodeling
- Stimulates the nervous system for better alertness, reflexes, and gastrointestinal movement
Triiodothyronine (T3) Hormone Production
The thyroid gland produces only about 20 percent of the body’s total T3 . The other 90 percent made from T4. This conversion occurs in various body tissues including the liver, kidney, and brain.
- Hyperthyroidism
- Hypothyroidism
- Quality of conversion in those on monotherapy T4 thyroid medications
Argument for Testing T3
Some proponents of t3 testing say there is no reason to test those with hypothyroidism. This is because some individual’s hypothyroid will have normal T3 levels.
Thyroid conditions may affect T3 levels before T4. That is why it is important to test T3 lab for a full picture of the thyroid.
T3 tests can be an indicator if thyroid medication is working properly. It can tell if T4 based medications are properly converting from T4 into T3 in the body. If T3 levels are low have your patient talk to their doctor about medications that can help stabilize their T3 levels.
Others will have reduced T3 levels as seen in those with chronic thyroid conditions as a byproduct of various drug interactions. Drug interactions can prevent T4 from being converted to T3 and result in low T3 levels.
Taking birth control pills can result in high levels of total T3. This is because the estrogens increase the level of the binding proteins.
Even just a 20 percent drop in T3 has been shown to double TSH while T4 remains the same. It is unclear if the hypothalamus, pituitary, or both was what stimulated the TSH.
In some individuals with a low TSH, only the T3 is elevated and the FT4 is normal.
Types of Triiodothyronine (T3)
There are two types of triiodothyronine:
- Total Triiodothyronine (Total T3)
- Free Triiodothyronine T3 (Free T3).
Total Triiodothyronine (Total T3)
Like total T4, total T3 is attached to a protein compound and transported through the body. About 99 percent of the T3 consists of total t3.
Free Triiodothyronine (Free T3)
The remaining one percent is unbound and flows freely through the body. This is the free T3. This type of T3 affects the HPT axis and thyroid hormone production.
Like T4, Free T3 is thought to be a better measure of thyroid function than Total T3.
T3 In Pregnancy
Physiological changes occur in pregnancy respectively. A study of women found different levels of T3 across trimesters:
- 1st Trimester 0.29-3.1 ng/100 mL
- 2nd trimester: 0.27-3.34 ng/100 mL
- 3rd Trimester, 0.24-3.61 ng/100 mL
Free T3 Optimal Thyroid Levels
Some integrative medical professionals argue that T3 levels are not optimal if they are not in the top half or even the top quarter of the reference range. This is something to have clients check with their doctor or endocrinologist about when getting test results.
Normal ranges for free triiodothyronine (Free T3) are as follows:
3 – 7 pmol/L (1.95 – 4.6 pg/mL)
Optimal thyroid levels of free T3 are as follows:
5 – 7 pmol/L (3.26 – 4.6 pg/mL)
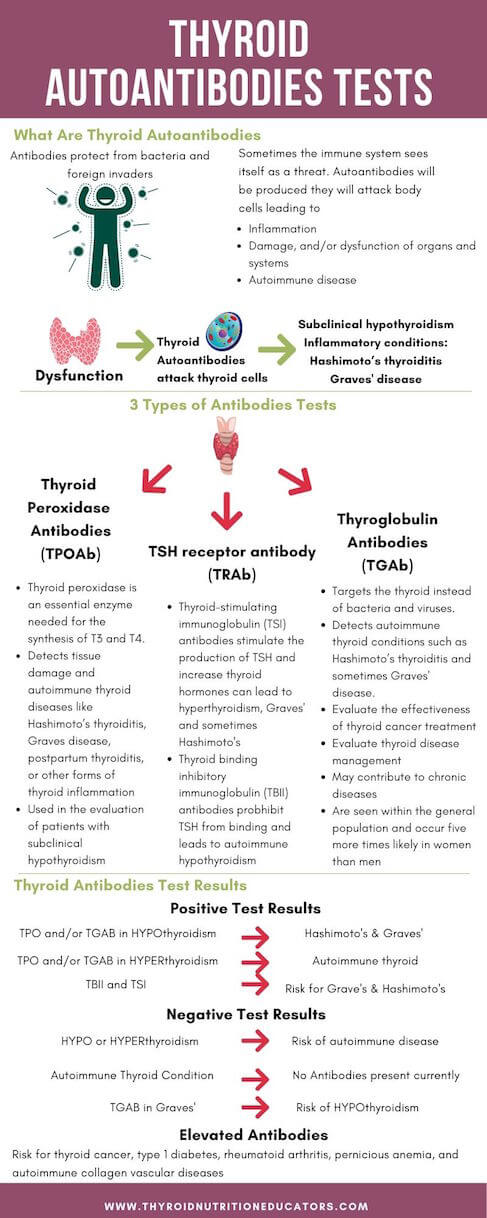
Thyroid Autoantibody Tests
The body’s defense against bacteria and foreign invaders are antibodies. Sometimes the immune system fails to tell the difference between itself and outside predators. When it sees itself as a threat autoantibodies will be produced.
Autoantibodies will attack their body cells. Inflammation, damage, and/or dysfunction of organs and systems will occur in response to this destruction. Autoimmune disease can also occur as a result of this immune response.
This is the case with thyroid disorders. Thyroid autoantibodies will see the thyroid cells as an antigen. Thyroid damage, inflammation of the thyroid, and other thyroid conditions will occur due to attacks from autoantibodies.
Thyroid autoantibodies can be present in many thyroid conditions including subclinical hypothyroidism, Hashimoto’s thyroiditis, and Graves’ disease.
The thyroid autoantibody tests show if thyroid autoantibodies are circulating in the blood. These tests help determine the health of the thyroid.
Three types of thyroid antibodies are found in the blood. They include the following:
- Thyroid peroxidase antibodies (TPOAb)
- Thyroglobulin antibodies (TGAb)
- TSH receptor antibody (TRAb)
Thyroid Peroxidase Antibody (TPOAb) Test
Thyroid peroxidase is an essential enzyme needed for the synthesis of T3 and T4.
The presence of TPO antibodies shows there is an autoimmunity present. The thyroid peroxidase antibody (TPOAb) test detects tissue damage and autoimmune thyroid diseases like Hashimoto’s thyroiditis, Graves disease, postpartum thyroiditis, or other forms of thyroid inflammation.
The presence of TPO antibodies increases the risk of developing thyroid disease.
The Whickham survey showed the likelihood of getting hypothyroidism increased by 2.1 percent per year based on the presence of TPO antibodies alone. When paired with an elevated TSH (greater than 6.0) the risk increased to 4.3 percent per year.
TPO antibodies are thought to be a secondary response to thyroid injury and may contribute to chronic diseases.
These antibodies are seen within the general population and occur five more times likely in women than men.
The presence of TPO antibodies shows a risk factor in families with autoimmune thyroid disorders.
TPOAb is also used in the evaluation of patients with subclinical hypothyroidism.
TPO Antibodies In Pregnancy
TPO antibodies often occur in women with recurrent miscarriages regardless of infertility. Women with positive TPO antibodies may be at risk for the following:
- Increased miscarriage in the first trimester
- Preterm delivery
- Impaired cognitive development of the fetus
TPOAb Optimal Thyroid Levels
The standard reference range of TPO antibodies is less than 9 IU/mL.
These antibodies can also be used to evaluate the management of thyroid disorders.
Use the optimal reference range to measure TPO antibodies:
- Less than 2 IU/mL
Thyroglobulin Antibody (TGAb) Test
Thyroglobulin (Tg) is a substance needed for the production of thyroid hormones T4 and T3. It is also where thyroid hormones and iodine are stored within the thyroid.
It is broken down and absorbed into thyroid cells during T3 and T4 secretion. Some small amounts of Tg are left intact and are sent out with T4 and T3. The remaining Tg is recycled back into thyroid cells so it can continue to create more thyroid hormones.
Thyroglobulin antibody (TGAb) is an antibody that targets the thyroid instead of bacteria and viruses.
Thyroglobulin antibody (TGAb) are used as a marker for the following:
- Autoimmune thyroid conditions such as Hashimoto’s thyroiditis and sometimes Graves’ disease.
- Evaluate the effectiveness of thyroid cancer treatment
- Evaluate thyroid disease management
Tg antibodies are thought to be a secondary response to thyroid injury and may contribute to chronic diseases. These antibodies are seen within the general population and occur five more times likely in women than men.
The presence of Tg antibodies shows a risk factor in families with autoimmune thyroid disorders.
Tg antibodies were the first antibody found in patients with autoimmune thyroid disease.
TGAb levels tend to be higher in those with an excessive iodine intake.
TG Antibodies and Thyroid Cancer
Some studies have suggested TGAb plays a role in the relationship between autoimmune thyroiditis and cancer. But the role autoantibodies indicating thyroiditis play in the progression of cancer is unclear.
TGAb appears in about 25 percent of patients with differentiated thyroid cancer. These antibodies occur about 1.5 times higher in those with cancer than the general population with benign nodules.
About one-fourth of patients who have thyroid cancer have antibodies to thyroglobulin. The presence of greater than 10 percent of Tg antibodies was also associated with recurrence of thyroid cancer in 25 percent of patients after a one year follow up. Cancer patients should have Tg antibodies checked at follow up visits.
The levels of thyroglobulin antibodies can mask thyroid cancer progression. Fluctuations in these antibodies levels can be used to monitor and evaluate cancer treatment. Decreases in Tg antibodies show the treatment is working. An increase in antibodies shows it is not effective.
TGAb Optimal Thyroid Levels
The standard reference range of TG antibodies is 0.5 to 43.0 ng/mL.
Use the optimal reference range to measure TG antibodies:
- Less than 2 IU/mL
Thyroid Stimulating Hormone Receptor Antibodies Tests
Thyroid-stimulating hormone receptor antibodies are antibodies that attack the TSH receptor.
These antibodies are responsible for thyroid growth and an increased rate of hormone production and secretion. It is what leads to a progression of thyroid disease, specifically autoimmune conditions.
These antibodies will show up in 90 percent of those with Graves’ disease and up to 20 percent of those with Hashimoto’s.
Thyroid-stimulating hormone receptor antibodies (TSHRAb) consist of 2 types of antibodies:
- Thyroid-stimulating immunoglobulin (TSI) antibodies
- Thyroid binding inhibitory immunoglobulin (TBII) antibodies.
Thyroid Stimulating Immunoglobulin (TSI) Antibodies
Thyroid-stimulating immunoglobulin (TSI) antibodies are an immunoglobulin that is mistaken for thyroid-stimulating hormone and binds to the TSH receptors on the thyroid gland. This will increase the production and secretion of T4 and T3.
The increase in thyroid hormones can result in hyperthyroidism and Graves’ disease.
Stimulatory antibodies have been found in 73 to 90 percent of Graves’ patients. The higher the levels of the antibodies the more active the Graves’ disease has become.
The presence of TSI antibodies does not automatically increase the risk for Graves’. About 50 percent of those with Hashimoto’s will also have periods of hyperthyroidism and present with TSI antibodies.
A small number of people with hypothyroid Hashimoto’s have developed hyperthyroidism associated with the appearance of TSI antibodies in addition to increased TgAb and TPOAb.
Thyroid Binding Inhibitory Immunoglobulin (TBII) Antibodies
Thyroid binding inhibitory immunoglobulin (TBII) antibodies block the action of the thyroid-stimulating hormone (TSH). They prevent TSH from binding to the cell membrane and leads to autoimmune hypothyroidism.
TBII antibodies are responsible for hypothyroidism and Hashimoto’s thyroiditis.TBII antibodies have also been found in Graves’ occurring in 25 to 75 percent of cases.
Hyperthyroidism and Graves’ can also develop in some hypothyroid patients due to TBII antibodies. This occurs in about 2 out of 34 patients (6%). It occurs in two ways:
- The unexpected development of TBII antibodies
- The process of thyroid damage from chronic thyroiditis overpowers the effects of TSIAb and eventually TSH
TSH blocking antibodies can be found in about 15 percent of those with autoimmune thyroiditis especially those with a goiter.
Measuring TBII antibodies is recommended before stopping hyperthyroid medications to learn if patients should be weaned off the medication.
Normal levels of TBIIAb indicate a better chance of remission. Relapse is associated with continuously high levels of these antibodies along with other measures identified in thyroid ultrasound. Assessment should be done more frequently after stopping hyperthyroid medications.
Those with mild disease, small goiters, and negative TBII antibodies have a greater than 50 percent remission rate. Hyperthyroid medications are often more favorable in this group.
TBII In Pregnancy Affect Fetal Development
Blocking antibodies may cause hypothyroidism and delayed development of the thyroid in newborns. TBII antibodies can cross the placenta and may lead to hyperthyroidism.
Pregnant women with hyperthyroidism should have TBII levels measured when the cause of the condition is unknown.
If it is Graves’ disease with elevated TBIIAb then the antibodies should be measured again at 22 to 26 weeks of pregnancy.
A woman treated for Graves’ with radioactive iodine or a thyroidectomy before pregnancy who becomes hypothyroid should have TBIIAb levels measured in the first trimester, then again at 20 to 26 weeks. This will indicate if the fetus can develop a thyroid condition.
Fluctuations of TSH Antibodies
Some patients can fluctuate between hyper- and hypothyroidism due to the presence of varying antibodies detected in the blood.
This is due to a higher concentration or a higher affinity for TSH stimulating antibodies over blocking antibodies. The research shows that concentrations of TBII antibodies that cause hypothyroidism need to be much higher than levels of TSI antibodies that induce hyperthyroidism.
Antibodies with the highest concentration may dominate and alter the thyroid condition.
Medications May Change The Concentration of TSHR Antibodies
Medications such as levothyroxine and antithyroid drugs may change the concentrations of autoantibodies.
A small number of hypothyroid patients positive for TBII antibodies were found to develop TSI antibodies and hyperthyroidism when treated with the thyroid medication levothyroxine.
A five-year survey showed treatment with antithyroid drugs such as methimazole lowers autoantibodies including TSI and TBII antibodies.
Six out of 26 people with Graves’ will develop hypothyroidism in association with TBII antibodies and a decrease in goiter after the withdrawal of anti-thyroid drugs used to treat Graves’.
Studies involving thyroid cells showed methimazole in high concentrations stopped the synthesis of autoantibodies agreeing with animal trials.
Hyperthyroid medication methimazole was found to prevent thyroid antibodies from forming in high concentrations both in vitro and in vivo. Other research shows hyperthyroidism medication can worsen autoimmunity.
Another study discredits drugs and says that recovering from hyperthyroidism helps to put a stop to the autoimmune disorder.
Medications work to give the body the thyroid hormone it is not making. Serum T4 may become elevated in some individuals resulting in TSI antibodies and hyperthyroidism.
TSH Receptor Antibodies Optimal Thyroid Levels
Reference ranges for TSH receptor antibodies vary depending on the lab. Below are some of the variations for TSI and TBII antibody tests.
TSI Antibodies Reference Ranges
The reference ranges for thyroid-stimulating hormone antibodies varies. Some lab values show it at less than or equal to 130 or 140 percent.
It has also been shown to be a range between 0 and 0.55 IU/L.
TBII Antibodies Reference Ranges
The reference range for thyroid-binding inhibitory immunoglobulin (TBII) antibodies is less than or equal to 16%.
Other lab values show a reference range between 1.5 and 1.75 IU/L or less.
- Healthy individual TBII: 1.22 IU/L
- Thyroid disease without a Graves’ diagnosis TBII: 1.58 IU/L
A study of TBII activity showed the following ranges:
- Normal controls: 0-6 %
- Graves’ disease: 55%
- Hashimoto’s thyroiditis: 10%
- Lymphocytic thyroiditis: 4.5%
- Postpartum thyroiditis: 5%
- Subacute thyroiditis 5%
Thyroid Antibodies Test Results
Thyroid Peroxidase (TPO) and Thyroglobulin antibodies (TGAb) are the most common antibodies to be tested. Having the addition of TSI and TBII antibodies is important for getting a clear picture of thyroid antibodies that may be present.
Positive Antibodies Test Results
POSITIVE test results with TPO and/or TGAb thyroid antibodies in the blood of a person with hypothyroidism mean they can have Hashimoto’s thyroiditis or Graves’ disease.
For a person with these antibodies and hyperthyroidism, they are likely to have autoimmune thyroid disease.
For those with Graves’ disease and elevated TGAb antibodies are at risk for hypothyroidism.
Negative Antibodies Test Results
NEGATIVE test results in someone with an under- or overactive thyroid condition can still be at risk for a thyroid autoimmune disease.
NEGATIVE test results do mean there are NOT any antibodies in your blood at the time of the test.
However, some individuals have autoimmune thyroid disease and will have no antibodies present in their blood.
Antibodies can develop over time. That is why it is important to continue to monitor the thyroid with a full antibody panel.
Elevated Antibodies Results
If your antibody levels are somewhat ELEVATED your client may be at risk for conditions like thyroid cancer, type 1 diabetes, rheumatoid arthritis, pernicious anemia, and autoimmune collagen vascular diseases.
Antibodies present point to an autoimmune disease. The higher the level of antibodies the more likely an autoimmune disease is present.
If thyroid antibodies are found in a pregnant woman this increases the risk of the baby developing hypo- or hyperthyroidism.
Antibodies Test Summary
While even some healthy people may have thyroid antibodies in their blood. Antibodies increase with age are and are higher in women. If you test positive for thyroid peroxidase antibodies, it may indicate an increased risk for thyroid disease and should be monitored over time to see if they become elevated.
Some argue testing antibodies is unnecessary in patients with existing thyroid conditions. This is ill-advised considering antibodies can measure further damage and remission of the thyroid.
It is also important to know how thyroid levels and if they are changing over time. A change in antibodies will indicate whether there is remission or if the condition is progressing over time.
Reverse Triiodothyronine (rT3)
Reverse Triiodothyronine or rT3 is a byproduct of the conversion of T4 to T3. Two types of T3 are derived from T4 by the removal of an iodine atom on a ring of carbon. Depending on where deiodination occurs will determine the type of T3 that is made:
- T3 is made when the carbon 5’ iodine is removed from the outer ring
- Reverse T3 is made when carbon 5 iodine is removed from the inner ring
Where T3 is the biologically active T3, reverse T3 is biologically inactive. Reverse T3 can attach to a thyroid receptor but cannot activate the hormone thus blocking the active T3 from binding.
Reverse T3 production is an evolutionary adaptation to protect the thyroid. It occurs in times of stress, physical trauma, injury, and illness T3 go down and rT3 levels will become elevated during the following conditions:
- Physical & emotional stress
- Chronic illness
- Chronic fatigue Syndrome
- Surgery
- Diabetes
- Heart disease
- Starvation
- Liver disease
- Kidney disease
- Certain cancers (breast, brain, colon)
Certain medications also elevate rT3 levels. They are as follows:
- Beta-blockers
- Amiodarone
- Ipodate and iopanoic acid
- Propylthiouracil
- Propranolol
- Dexamethasone
In regards to thyroid conditions, reverse T3 has shown the following patterns:
Controversy Over Reverse T3 Testing
There is some controversy over the testing of rT3. Some medical professionals say it is not a valid test. On the other hand, rT3 is of interest to functional integrative healthcare professionals.
They feel that rT3 testing can signal rt3 dominance. Reverse T3 dominance is when rT3 competes with T3 at binding sites resulting in elevated rt3.
People with rT3 dominance will experience hypothyroid symptoms even with normal T3 levels. Checking for rt3 is a way to tell if a medication is converting properly from T4 to T3.
Other thyroid experts say checking T4 and T3 levels is a better way to tell if medication is working.
Reverse T3 Optimal Thyroid Levels
If your clients have normal T3 levels but still suffer from low energy and poor metabolism you may want to check RT3 levels.
Reverse T3 normal reference ranges are as follows:
- 9.2−24.1 ng/dL
Reverse T3 optimal thyroid levels:
- 11-18 ng/dl
According to functional medicine, a healthy range will be the bottom three numbers of any provided range.
Some practitioners will also look at different ratios involving T3 and rT3 such as the following
- Total T3/rT3 which should be 10 or higher
- Free T3/rT3 which should be 20 or higher
- rT3/Free T3 which should be less than 10:1

Thyroid Ultrasound
There is the case that bloodwork does not show a pattern for thyroid disease. That is where the thyroid ultrasound comes in. This is a common and useful way to image the thyroid when blood work does not give clear answers about the health of the thyroid.
The ultrasound will have a high sensitivity for detecting nodules. Thyroid nodules are lumps in your neck. It will indicate if the nodule is caused by a thyroid condition, iodine deficiency, or is benign. Thyroid conditions include:
Ultrasound technology has been able to discover thyroiditis or Graves’ disease among 55 patients (29 with Graves’ disease and 26 with toxic nodules) [R].
Thyroid Symptoms
Another thing to take into consideration is a client’s symptoms. This can tell a lot about what is going on with their thyroid. There are a ton of symptoms for both hypo- and hyperthyroid conditions. If there are no symptoms the thyroid could be in a better state of health. Though this is not always the case.

Thyroid Hormone Lab Values for Various Thyroid Conditions
Each thyroid condition will have different lab values. Here is a cheat sheet to give insight into what condition may be affecting your client.
Euthyroid: Normal Labs & Physical Thyroid Symptoms
The blood work comes back normal but someone is still having physical thyroid symptoms. A client can still be at risk for thyroid disease.
Parameters for euthyroid:
- TSH – Normal
- Free T3 – Normal or low
- rT3 – Elevated
- Free T4 – Normal
- TPO Antibodies – Negative
- TG Antibodies – Negative
There could also be normal or there could be a decreased conversion of T4 to T3. Antibody tests will be negative.
You want to double-check to see the levels are optimal and not within “normal” reference ranges.
Since T3 looks normal testing rT3 can indicate if there is a problem going on. An ultrasound may also be helpful. If these come back normal checking adrenals is the next step.
Euthyroid Sick Syndrome: Low T3, Normal/Low T4, Elevated rT3
The most common hormone pattern in sick euthyroid syndrome is as follows:
- Free T3 – Low
- Free T4 – Normal to low
- TSH – Normal
- rT3 – Elevated
Other times in euthyroid sick syndrome there can be the following:
- Free T4 – Low
- Free T4 & T3 – Low
- Free T4 – Elevated
- TPO Antibodies – Positive
- TG Antibodies – Positive or Negative
The most common abnormality is low T3. Low free T4 is seen in a bad prognosis.
Central Hypothyroidism
Central hypothyroidism is hypothyroidism that occurs due to a problem with the hypothalamus or pituitary gland.
Most people have normal or low TSH levels so using TSH alone can delay or miss a central hypothyroidism diagnosis. Slightly high TSH levels have also been seen in some cases of central hypothyroidism.
Central hypothyroidism levels include the following:
- TSH: Normal or Low
- Free T3: Low
- Free T4: Low
- TPO Antibodies – Positive or Negative
- TG Antibodies – Positive or Negative
Euthyroid Hashimoto’s
Euthyroid Hashimoto’s is when there is enough thyroid hormone but autoimmunity is still taking place.
Euthyroid Hashimoto’s levels include the following [R]:
- TSH – Normal
- Free T3 – Normal
- Free T4 – Normal
- TPO Antibodies – Positive
- TG Antibodies – Positive
Those with deteriorating thyroid function often have higher TG antibodies.
Euthyroid Hashimoto’s is also considered stage 2 of Hashimoto’s.
Subclinical Hypothyroidism
Subclinical hypothyroidism is also known as mild thyroid failure is when the thyroid is losing the ability to produce thyroid hormone. In this condition, TSH levels are mildly elevated while T3 and T4 are normal.
Subclinical hypothyroidism features:
- TSH – Mildly elevated
- FREE T3 – Normal
- FREE T4 – Normal
- TPO Antibodies – Positive or Negative
- TG Antibodies – Positive or Negative
Subclinical hypothyroidism is also known as stage 2 of Hashimoto’s when the antibodies are positive. Even if no antibodies are present the thyroid can still be under-active. Getting an ultrasound will show evidence of Hashimoto’s.
Overt Hypothyroidism
Overt hypothyroidism is the point when the thyroid gland is no longer able to produce enough thyroid hormone. The thyroid is underactive and the body cannot run as it normally does due to too little thyroid hormone in the blood.
Overt hypothyroidism features:
- TSH – Elevated
- Free T3 – Low
- Free T4 – Low
- TPO Antibodies – Positive or Negative
- TPG Antibodies – Positive or Negative
This is also known as stage 4 of Hashimoto’s especially if antibodies are positive. Those with seronegative Hashimoto’s may not have any antibodies present but the thyroid is still being attacked. An ultrasound can distinguish whether or not it is Hashimoto’s.
Subclinical Hyperthyroidism
Subclinical hyperthyroidism is when the pituitary gland tells the thyroid to make less hormone. TSH will be low but hormone levels will be normal. There also may or may not be the presence of antibodies. This is the condition that occurs before overt hyperthyroidism.
Subclinical hyperthyroidism features:
- TSH – Low
- Free T4 – Normal
- Free T3 – Normal
- TPO Antibodies – Positive or Negative
- TG Antibodies – Positive or Negative
If Graves’ disease is suspected testing for TSI and TBII antibodies is recommended.
Some patients with autoimmune hypothyroidism also have evidence of either TBII or, but rarely, TSI antibodies.
TSHR autoantibodies may be detected before autoimmune thyrotoxicosis occurs.
Overt Hyperthyroidism
Overt hyperthyroidism is when there is too much thyroid hormone being produced. The thyroid is considered overactive. Thyrotoxicosis is another name for hyperthyroidism.
Overt hyperthyroidism features:
- TSH – Low
- Free T4 – Elevated
- Free T3 – Elevated
- TPO Antibodies – Positive or Negative
- TG Antibodies – Positive or Negative
- TSI Antibodies – Positive or Negative
- TBII Antibodies – Positive or Negative
TSH will be low and hormones will be elevated. This can include either T4 and T3 or both.
There are a few types of overt hyperthyroidism:
- Graves’ disease
- Multinodular goiter
- Autonomously functioning thyroid nodules (AFTN)
Graves’ Disease
Fifty to 90 percent of Graves’ disease patients will have the presence of Tg and TPO antibodies.
Those with Graves’ disease may also have TBII antibodies. The balance between TSI and TBII is a good indicator of a Graves’ relapse after antithyroid drug treatment withdrawal. TSI antibodies were a better predictor of relapse than TBII antibodies.
Multinodular Goiter (MNG)
Multinodular goiter (MNG) is when there is more than one nodule on the thyroid. It is a common genetic disorder that causes irregular thyroid cells.
The diagnosis is based on physical examination. It is often detected as a mass in the neck but sometimes an enlarging gland can also produce symptoms. Imaging procedures are also useful.
MNG thyroid function tests may indicate the following:
- Normal thyroid levels
- Subclinical hyperthyroidism
- Overt hyperthyroidism
MNG can also develop into hyperthyroidism after a few decades usually due to excess iodine.
Autonomously Functioning Thyroid Nodules (AFTNs)
An autonomous functioning thyroid nodule (AFTN) is a localized nodular lesion on the thyroid. It is evaluated by its growth iodine update, and function.
These nodules are common and can result from different factors:
- Genetics may be responsible for cell growth
- Environmental factors like iodine deficiency or other goitrogens
Since TSH does not control nodules they are considered autonomous. TSH levels can be normal, low, or elevated in this condition:
Thyroid scanning is recommended since thyroid tests cannot indicate AFTN.
AFTN are problematic if they become toxic. Surgery or radioiodine are typical treatments.
Continuously Monitor The Thyroid
Screening for optimal thyroid levels should be made part of every annual health examination. If your client has not had a thyroid screening now is the time to get it.
Their medical doctor can order a test or they can get a complete thyroid panel test from Ulta Labs.
If results show thyroid levels are out of optimal range you should work with their endocrinologist so you both can craft a medication and nutrition plan specific to their needs.
Those with Thyroid Conditions Must Monitor The Thyroid
Those with existing thyroid conditions should get monitored every 4 to 6 months to evaluate the health of the thyroid.
Summary
Getting a complete thyroid panel is important for understanding the health of the thyroid. Find out how functional nutrition can help support thyroid health as well.

More Nutrition Thyroid Articles
- Functional Nutrition for Thyroid
- Best Foods for Thyroid Patients
- Alcohol and the Thyroid
- Should Your Clients go Gluten Free
- Mushroom Supplements for Thyroid Nutrition
- Infrared Sauna Benefits
- Mock Meat and the Thyroid
- Signs of a Thyroid Condition
- Probiotics for Thyroid Health
- Thyroid and Eczema
The information on this website has not been evaluated by the Food & Drug Administration or any other medical body. It is shared for educational purposes only and is not intended to diagnose, treat, prevent, or cure any disease. Consult your doctor or healthcare provider before making changes to your diet, exercise regimen or lifestyle. By accessing or using this website, you agree to abide by the Terms of Service, Full Disclaimer, and Privacy Policy. Content may not be reproduced in any form.


Pingback: Best Food for Thyroid Patients - Thyroid Nutrition Educators
Pingback: Essential Oils for Thyroid Health - Thyroid Nutrition Educators
Pingback: Should Your Thyroid Remedies Include A Gluten Free Lifestyle? - Thyroid Nutrition Educators